- Bone Health
- Immunology
- Hematology
- Respiratory
- Dermatology
- Diabetes
- Gastroenterology
- Neurology
- Oncology
- Ophthalmology
- Rare Disease
- Rheumatology
AbbVie's Gonzalez Is on Defense as House Members Petition FTC
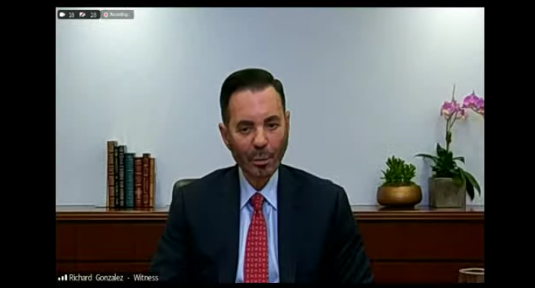
Accused of unfair trade practices, AbbVie's CEO Richard Gonzalez pointed the finger at Medicare Part D.
Various House members have asked the Federal Trade Commission (FTC) to open an antitrust investigation into pharmaceutical giant AbbVie, which allegedly has exceeded its patent rights in preventing biosimilar competition to arthritis drug Humira (adalimumab) in the United States.
The request follows the release of a report from the House Committee on Oversight and Reform that outlines attempts by AbbVie to prevent competition and thereby reap $107 billion in US revenues alone since 2003. Biosimilar competitors have attempted to enter the US market but have been delayed until 2023 by AbbVie litigation and negotiated settlements.
“We make this request in light of previously non-public documents obtained by the Committee on Oversight and Reform during its multi-year investigation of AbbVie,” the members wrote.
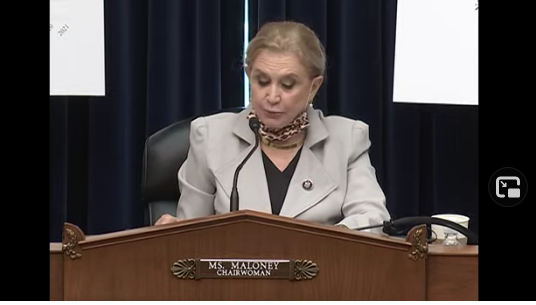
“Based on our review, these documents indicate that AbbVie delayed biosimilar competition for far longer than warranted by its own internal evaluations of the strength of its patent portfolio, which anticipated biosimilar entry no later than 2017.” The FTC request was authored by Representatives Carolyn B. Maloney, D-New York, chairwoman of the Committee on Oversight and Reform; Jerrold Nadler, D-New York, chairman of the Committee on the Judiciary; and David N. Cicilline, D-Rhode Island, chairman of the Committee on the Judiciary’s Subcommittee on Antitrust, Commercial, and Administrative Law.
A Daylong Hearing
The request preceded a daylong hearing involving testimony and inquiry into AbbVie’s pricing and marketing practices, during which AbbVie CEO Richard Gonzalez also testified. Audience members heard expert opinion and also commentary from patients who said that AbbVie’s pricing policies for Humira had placed this drug beyond their reach or forced them to make very difficult tradeoffs. The report stated that AbbVie now charges roughly $77,000 for an annual supply of Humira, 470% higher than when the drug was launched in 2003.
Katherine Pepper, of Bellingham, Washington, said she suffers from debilitating pain and reduced mobility caused by psoriatic arthritis. She was prescribed twice-weekly Humira injections, costing $5900 for a pack of 2 injection pens. “Even as a Medicare beneficiary on a fixed income, I still have to pay nearly $1200 out of pocket every single month,” she said. “I can’t afford this. I don’t know any average person who can. The excessive Humira price forces me to choose every month whether to eat or fill my prescriptions. This company’s price gouging needs to stop,” she said.
For an overview of the House committee’s investigative report on AbbVie, which reviewed 170,000 pages of internal company documents, click here.
In his testimony, Gonzalez stated that much of AbbVie’s revenues go toward research and development into new products that might yield substantial benefit for patients—$50 billion since 2013. “As we tackle the issues of drug pricing and access, it’s important that we focus on what’s working and what needs to change to make sure that patients get the medicines they need,” he said.
Medicare Part D
Gonzalez said a major culprit for the payment gap suffered by patients is the Medicare Part D program, which he said fails to cover drugs costs adequately. “For these patients, reducing drug prices alone will not alleviate the challenge of access and affordability,” he said.
“What’s not working in Part D is that some patients must bear too much of the out-of-pocket cost, and there’s no cap on drug spending. Part D enrollees cannot access co-pay support, they cannot purchase insurance to defray these costs, and they must pay open-ended drug expenses. The average out-of-pocket cost is almost 100 times higher for a medicine like Humira than any other US patient group. No other prescription drug insurance program puts so much cost burden on the patient,” he said.
AbbVie does have a patient assistance program, and 1 out of 3 patients in Part D are seeking assistance or receiving free medicine, he said. This “stands in stark contrast” to commercially insured Humira patients. One out of 100 seek assistance from the AbbVie patient assistance program, he said. “Medicare Part D patients’ out-of-pocket costs are the single biggest issue when it comes to drug affordability.”
Newsletter
Where clinical, regulatory, and economic perspectives converge—sign up for Center for Biosimilars® emails to get expert insights on emerging treatment paradigms, biosimilar policy, and real-world outcomes that shape patient care.