- Bone Health
- Immunology
- Hematology
- Respiratory
- Dermatology
- Diabetes
- Gastroenterology
- Neurology
- Oncology
- Ophthalmology
- Rare Disease
- Rheumatology
Experts Pressure Congress to Remove Roadblocks for Biosimilars
Lawmakers and expert witnesses emphasized the potential of biosimilars to lower health care costs by overcoming barriers like pharmacy benefit manager practices, limited awareness, and regulatory delays to improve access and competition in chronic disease management during a recent congressional hearing.
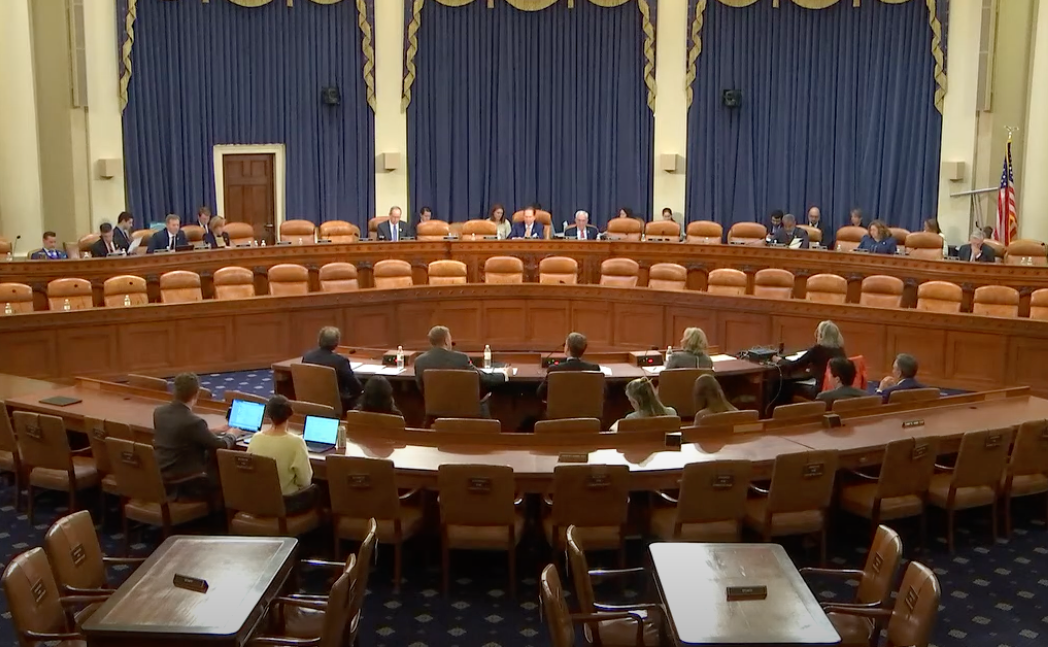
The experts invited to testify are seated at the large table in front of the Committee members. From left to right: Aaron S. Kesselheim, MD, JD, MPH, Craig Burton, Colin C. Edgerton, MD, and Debra Patt, MD, PhD, MBA.
As chronic diseases continue to drive 90% of the nation’s $4.5 trillion in annual health care spending, expanding access to lower-cost biosimilars emerged as a critical solution in a recent congressional hearing on lowering health care costs and improving patient access.1
Lawmakers from the House Committee on Ways and Means and 4 expert witnesses highlighted the $23.6 billion in savings already generated by biosimilars since their introduction in 2015, while calling attention to the barriers that continue to limit their use, such as restrictive reimbursement practices and limited provider and patient awareness. The hearing also explored policy reforms to streamline biosimilar approvals, promote competition, and support innovation, emphasizing the potential of biosimilars to transform chronic disease management and improve outcomes for millions of Americans.
The 4 witnesses included:
- Debra Patt, MD, PhD, MBA, a medical oncologist at TexasOncology2
- Colin C. Edgerton, MD, a rheumatologist at Articularis Healthcare Group and a member of the American College of Rheumatology ultrasound task force3
- Craig Burton, executive director of the Biosimilars Council and a member of The Center for Biosimilars® Advisory Board4
- Aaron S. Kesselheim, MD, JD, MPH, a professor of medicine at Harvard Medical School and director of the Program on Regulation, Therapeutics, and Law within the Division of Pharmacoepidemiology and the Pharmacoeconomics Department of Medicine at Brigham and Women’s Hospital5
Patt kicked off the expert testimonies, bringing attention the transformative role biosimilars play in improving affordability and access to cancer treatment.1 She shared her experience as an oncologist at Texas Oncology, where biosimilars have been successfully integrated into care for over a decade, noting that these medications are just as safe and effective as their reference biologics but are significantly more affordable for patients. Despite their clinical benefits, Patt emphasized the systemic barriers that hinder biosimilar adoption—namely, distorted market forces driven by pharmacy benefit managers (PBMs) and the 340B Drug Pricing Program.
Patt criticized PBMs for manipulating formulary access based on profitability rather than patient benefit, often favoring more expensive originator biologics or private-label biosimilars that provide them with greater rebates. This practice not only limits physician autonomy but also undermines the affordability and viability of biosimilars.
“This practice creates a financial environment where there are drivers that incentivize the utilization of more expensive biologics or ‘private label’ biosimilars rather than lower-cost biosimilars. And, as we have seen average sales price drop precipitously for biosimilars, oncology and other specialty practices may increasingly be underwater—that is, reimbursement lower than acquisition cost—for biosimilar products, making their selection an unsustainable solution,” Patt explained.2
Additionally, she explained how 340B hospitals—despite their nonprofit status—are incentivized to use higher-cost originator biologics to maximize revenue, further distorting the drug market and discouraging biosimilar use.1
She recommended several reforms to promote biosimilars, including streamlining their regulatory approval process, eliminating PBM rebates on biosimilars, and increasing reimbursement rates to ensure financial sustainability. She also called for a price floor for biosimilars to prevent supply chain disruptions.
Edgerton’s testimony emphasized the significant, yet underutilized, potential of biosimilars to reduce prescription drug spending and increase access to essential treatments in the US health care system. Despite being scientifically sound and FDA approved, biosimilars face slow adoption due to structural barriers, especially the role of PBMs and health plan incentives, such as reimbursements. These intermediaries often favor high-cost originator biologics that offer larger rebates, excluding biosimilars from formularies or placing them in higher cost-sharing tiers.
“The gap between the cost of acquiring biosimilar treatments for administration to patients, and the amount we are reimbursed upon administering those treatments is negatively impacting both physician practices and access to care for millions of patients suffering from chronic diseases,” Edgerton emphasized.3
To address these challenges, Edgerton called for increased transparency in rebate and PBM practices, reforms to prevent anticompetitive contracting by brand manufacturers, and the federal authority to negotiate drug prices, particularly in Medicare.1 He also stressed the importance of provider and patient education to build confidence in biosimilars. These policy changes, he argued, are essential to create a competitive market that supports biosimilar adoption and improves affordability for patients.
Burton highlighted a troubling slowdown in biosimilar development, underscored by a recent IQVIA report that revealed a stark gap: Of the 62 reference biologics expected to lose patent exclusivity by the end of 2024, only 14 had biosimilars in development.1,6
This means 90% of potential biosimilar opportunities are currently being missed—representing a critical loss for patients who depend on more affordable treatments.6 Burton pointed to significant consequences for Medicare patients, particularly the 860,000 with diabetes, 102,000 with neurological conditions such as multiple sclerosis, and 160,000 with immunological diseases, all of whom could benefit from lower-cost biosimilars.1
Burton cited barriers across the biosimilar lifecycle, including FDA requirements for costly trials, delays from patent thickets, insurer and PBM favoritism toward branded drugs, and Medicare reimbursement disincentives. He also criticized the Inflation Reduction Act (IRA) for misaligning price negotiation timelines with the lengthy biosimilar development cycle.7 For example, price controls may be triggered before biosimilars even reach the market, undermining competition and investment.
“If nothing changes, patients and the health care system will pay the price…This isn’t just a theoretical discussion; it’s a crisis that will impact real people: the diabetic patient struggling to afford their insulin, the cancer survivor burdened by high treatment costs, the retiree on a fixed income choosing between life-sustaining medicines and rent,” Burton warned.4
Kesselheim’s testimony emphasized that US patients, especially seniors on Medicare, pay more for brand name drugs than those in other high-income countries, often leading to poor health outcomes. He outlined key several steps to improve access, including protecting public investment in research and strengthening the IRA.1
The hearing was held by the House Subcommittee on Health, which is within the Committee on Ways & Means. | Image credit: Philip - stock.adobe.com

The professor emphasized that nearly all significant pharmaceutical innovations in recent decades have relied on substantial public funding, especially from the National Institutes of Health (NIH). He warned that since the second Trump administration began, the rate of new NIH grants has dropped to less than half the amount awarded during the same period in 2024.8 He urged Congress to restore normal funding levels to avoid long-term damage to the US scientific enterprise and future innovation.5
“These funding cuts threaten innovation across all fields of medicine, including HIV and Alzheimer’s disease... The erosion of funding not only undermines opportunities for scientific discovery in the short-term, but it also threatens advances that could benefit future generations, as young scientists are driven out of research careers in the US.”
He also noted that early negotiations under the IRA for the first 10 selected medicines have already led to major price reductions and are projected to save $100 billion.1 Kesselheim stressed that weakening IRA provisions, such as drug price negotiations and out-of-pocket caps, could undercut savings without benefiting patients. He ended with stressing the need for congressional leaders to take more action promote biosimilar competition.
“Congress should advance laws that ensure the long-term affordability of biologic drugs, such as making it harder for manufacturers to build large thickets of biologic patents that block timely biosimilar entry, enacting restrictions on pharmaceutical benefit manager drug rebate flexibilities to enhance insurer coverage of lower-cost biosimilar drugs, and changing CMS rules to allow common billing codes for biologics and biosimilars.”5
References
1. Health Subcommittee Hearing on Lowering Costs for Patients: The Health of the Biosimilar Market. US House Committee on Ways & Means. April 8, 2025. Accessed April 11, 2025. https://waysandmeans.house.gov/event/health-subcommittee-hearing-on-lowering-costs-for-patients-the-health-of-the-biosimilar-market/
2. Health Subcommittee Hearing on Lowering Costs for Patients: The Health of the Biosimilar Market; Committee on Ways & Means, 119th Cong (2025) (testimony of Debra Patt, MD, PhD, MBA, medical oncologist, at TexasOncology). Accessed April 11, 2025. https://waysandmeans.house.gov/wp-content/uploads/2025/04/Patt-Testimony-1.pdf
3. Health Subcommittee Hearing on Lowering Costs for Patients: The Health of the Biosimilar Market; Committee on Ways & Means, 119th Cong (2025) (testimony of Colin C. Edgerton, MD, rheumatologist, Articularis Healthcare Group; director, American College of Rheumatology ultrasound task force). Accessed April 11, 2025. https://waysandmeans.house.gov/wp-content/uploads/2025/04/Edgerton-Testimony-1.pdf
4. Health Subcommittee Hearing on Lowering Costs for Patients: The Health of the Biosimilar Market; Committee on Ways & Means, 119th Cong (2025) (testimony of Craig Burton, executive director, Biosimilars Council). Accessed April 11, 2025. https://biosimilarscouncil.org/wp-content/uploads/2025/04/04042025-FINAL-Biosimilars-Hearing-Testimony.pdf
5. Health Subcommittee Hearing on Lowering Costs for Patients: The Health of the Biosimilar Market; Committee on Ways & Means, 119th Cong (2025) (testimony of Aaron S. Kesselheim, MD, JD, MPH, professor of medicine, Harvard Medical School; director, Program on Regulation, Therapeutics, And Law, the Division of Pharmacoepidemiology and the Pharmacoeconomics, Department of Medicine, Brigham and Women’s Hospital). Accessed April 11, 2025. https://waysandmeans.house.gov/wp-content/uploads/2025/04/Kesselheim-Testimony-1.pdf
6. Jeremias S. The biosimilar void: 90% of biologics coming off patent will lack biosimilars. The Center for Biosimilars. February 5, 2025. Accessed April 11, 2025. https://www.centerforbiosimilars.com/view/the-biosimilar-void-90-of-biologics-coming-off-patent-will-lack-biosimilars
7. Jeremias S. CMS announces new drug prices under the IRA, including for Stelara and Enbrel. The Center for Biosimilars. August 19, 2024. Accessed April 11, 2025. https://www.centerforbiosimilars.com/view/cms-announces-new-drug-prices-under-the-ira-including-for-stelara-and-enbrel
8. Kazlov M, Ryan C. How Trump 2.0 is slashing NIH-backed research — in charts. April 10, 2025. Updated April 11, 2025. Accessed April 11, 2025. https://www.nature.com/articles/d41586-025-01099-8
Newsletter
Where clinical, regulatory, and economic perspectives converge—sign up for Center for Biosimilars® emails to get expert insights on emerging treatment paradigms, biosimilar policy, and real-world outcomes that shape patient care.
