- Bone Health
- Immunology
- Hematology
- Respiratory
- Dermatology
- Diabetes
- Gastroenterology
- Neurology
- Oncology
- Ophthalmology
- Rare Disease
- Rheumatology
Manitoba Adopts Biosimilar Switching Policy
Manitoba’s new policy means that all 10 Canadian provinces now have an initiative to boost biosimilar adoption and savings by transitioning patients on reference agents to biosimilar options.
The Government of Manitoba has announced the implementation of a biosimilars transition policy to expand the use of biosimilar medicines and generate savings.1 The new policy means that all 10 Canadian provinces now have a policy of this nature.
Manitoba is Canada's fifth most populated province.10 Winnipeg, pictured above, is the capital and the sixth most populous municipality in Canada.
Image credit: Jacob - stock.adobe.com

“Biosimilars Canada and its member companies congratulate Deputy Premier and Health Minister Uzoma Asagwara and the Government of Manitoba for implementing a biosimilars switching policy to provide patients with access to the high-quality treatments and support services they need while also generating significant ongoing savings for Manitoba’s healthcare system,” said Jim Keon, president of Biosimilars Canada in a statement.2
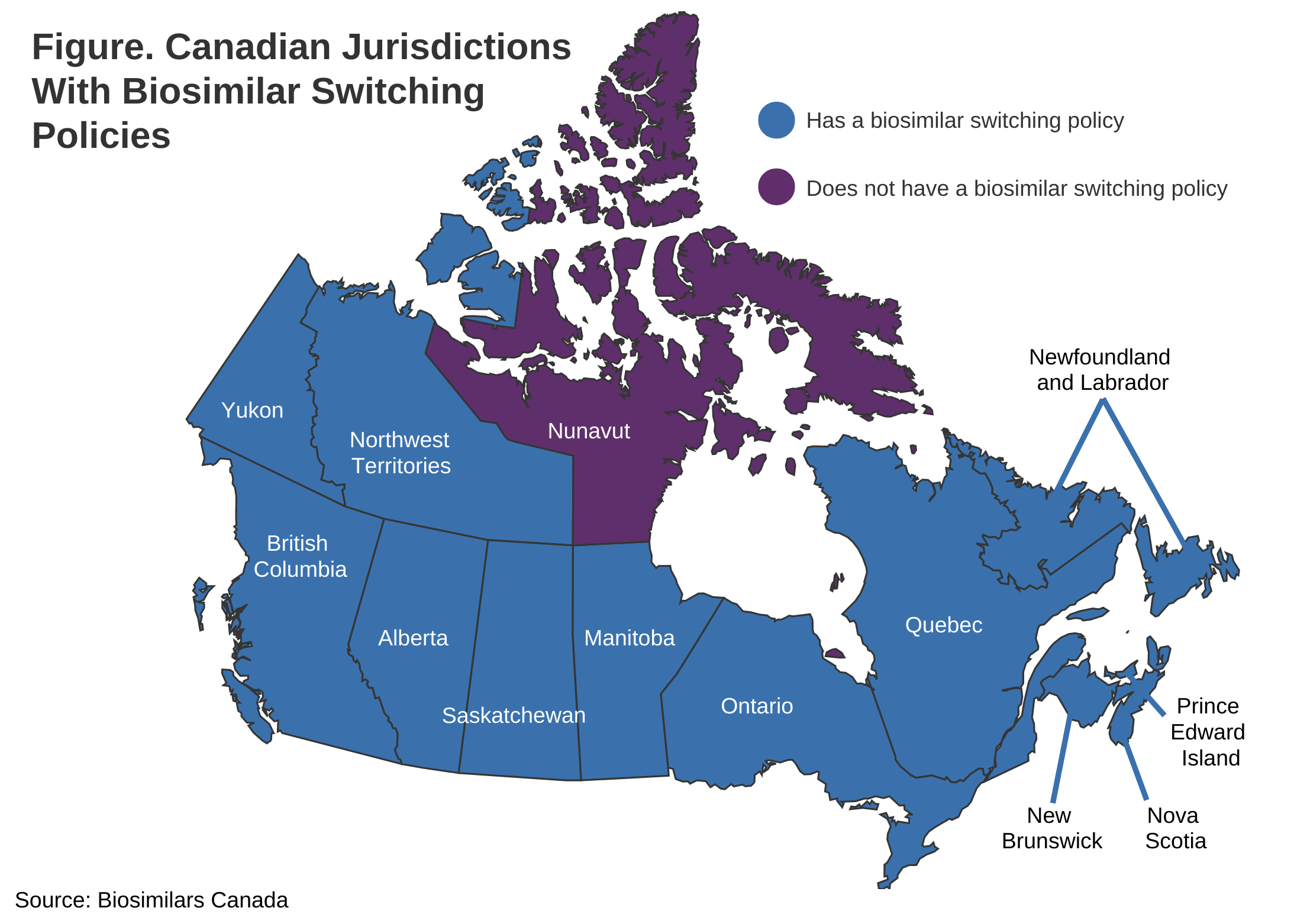
The Manitoba implementation follows British Columbia (May 2019), Alberta (December 2019), New Brunswick (April 2021), Quebec (July 2021), Nova Scotia (February 2022), Saskatchewan (October 2022), Ontario (December 2022), Newfoundland and Labrador (March 2023), and Prince Edward Island (October 2023). Two Canadian territories have also adopted biosimilar transition initiatives: the Northwest Territories (December 2021) and Yukon Territory (April 2023). (Figure)
Similar to other provinces, Manitoba’s initiative features a transition period. If a patient is currently using 1 of the 10 reference biologics listed by the Manitoba government, they will need to switch to a biosimilar version by January 31, 2025, to maintain coverage under Pharmacare or other provincial plans. During the transition period, both the reference biologic and biosimilars will be covered, allowing time for patients to consult their healthcare providers and obtain new prescriptions.
Of the 13 jurisdictions in Canada, 12 now have biosimilar switching policies. Nunavut, which has a mostly indigenous population and is the least populated jurisdiction, is the only one remaining.
After the transition period, the 10 reference biologics will no longer be covered, unless a suitable biosimilar is unavailable. Patients can request exceptions for continued coverage if a suitable biosimilar cannot be used for medical reasons, with requests reviewed on a case-by-case basis.
The reference agents losing coverage at the end of the transition period include Humira (adalimumab), Lovenox (enoxaparin), Enbrel (etanercept), Neupogen (filgrastim), Copaxone (glatiramer), Remicade (infliximab, NovoRapid (insulin aspart), Lantus (insulin glargine), Humalog (insulin lispro), and Rituxan (rituximab).
Transitioning from originators biologics to biosimilars is safe and common, particularly throughout Europe, where regulatory agencies in the European Union and United Kingdom have declared all biosimilars as interchangeable with their reference agents upon approval.3,4
Additionally, several reviews have boasted the safety of switching between reference products and biosimilars without impacting clinical outcomes.5,6 However, researchers warn about the nocebo effect, where patients’ negative thoughts about a biosimilar can lead to worsened clinical outcomes.7
One observational study of patients in Canada with inflammatory bowel disease undergoing mandatory switching to an infliximab or adalimumab biosimilar found that while there were no changes in clinical remission or antidrug antibodies after 24 weeks, 13% of patients experienced the nocebo effect, leading to one-fifth of those patients discontinuing biosimilar therapy.8 The authors wrote, “The nocebo effect is “an important clinical concern in the current era of biosimilars, since it has a detrimental influence on drug adherence, patient quality of life, and treatment outcomes.”
Transition policies have also shown to be effective in generating savings for Canadian provinces. British Columbia recently published a report showing that transitioning 40,000 patients from reference products to biosimilars during the first 5 years of its biosimilar transition initiative saved the province $732 million while maintaining comparable health outcomes.9 The savings were able to be reinvested to improve British Columbia’s public payer program.
Biologic medicines, crucial for treating serious diseases, can be very expensive, costing between $10,000 and $25,000 per patient annually, which strains drug budgets. Biosimilars Canada said that to fully benefit from biosimilars, drug plans need to adopt policies that support their use through effective transitioning or "switching" strategies.
Extensive real-world data supports the use of biosimilars. In Canada, biosimilars account for 2.69 million retail prescriptions annually and are widely used in hospitals and oncology programs. Additionally, over 178 clinical trials with around 21,000 switched patients have shown that switching from originator biologics to biosimilars does not lead to significant issues in efficacy, safety, or immunogenicity.
References
1. Manitoba biosimilars initiative. Manitoba government. Accessed August 6, 2024. https://maps2.gov.mb.ca/health/pharmacare/biosimilars.html
2. Manitoba announces transition to cost-saving biosimilar medicines. Biosimilars Canada. Press release. August 6, 2024. Accessed August 6, 2024. https://biosimilarscanada.ca/blog/manitoba-announces-transition-to-cost-saving-biosimilar-medicines/
3. Statement on the scientific rationale supporting interchangeability of biosimilar medicines in the EU. European Medicines Agency. April 21, 2023. Accessed August 6, 2024. https://www.ema.europa.eu/en/documents/public-statement/statement-scientific-rationale-supporting-interchangeability-biosimilar-medicines-eu_en.pdf
4. Guidance on the licensing of biosimilar products. UK government. Updated November 7, 2022. Accessed August 6, 2024. https://www.gov.uk/government/publications/guidance-on-the-licensing-of-biosimilar-products/guidance-on-the-licensing-of-biosimilar-products#:~:text=5.-,Interchangeability,achieve%20the%20same%20therapeutic%20effect
5. Ferreri D. Analyzing safety of switching from originators to biosimilars: A meta-analysis of 21 trials. The Center for Biosimilars®. February 10, 2024. Accessed August 6, 2024. https://www.centerforbiosimilars.com/view/analyzing-safety-of-switching-from-originators-to-biosimilars-a-meta-analysis-of-21-trials
6. Jeremias S. Study on nonmedical switching for adalimumab biosimilars warns about nocebo effect. The Center for Biosimilars. April 27, 2023. Accessed August 6, 2024. https://www.centerforbiosimilars.com/view/study-on-nonmedical-switching-for-adalimumab-biosimilars-warns-about-nocebo-effect
7. Jeremias S. Switching Patterns highlight nocebo effect in European patients using Amgevita. The Center for Biosimilars. July 23, 2024. Accessed August 6, 2024. https://www.centerforbiosimilars.com/view/switching-patterns-highlight-nocebo-effect-in-european-patients-using-amgevita
8. Ferreri D. Patients with IBD experience nocebo effect post mandatory switch to biosimilar. The Center for Biosimilars. May 11, 2024. Accessed August 6, 2024. https://www.centerforbiosimilars.com/view/patients-with-ibd-experience-nocebo-effect-post-mandatory-switch-to-biosimilar
9. Jeremias S. British Columbia’s biosimilar switching program saves $732 million in 5 years. The Center for Biosimilars. June 18, 2024. Accessed August 6, 2024. https://www.centerforbiosimilars.com/view/british-columbia-s-biosimilar-switching-program-saves-732-million-in-5-years
10. Population and dwelling counts: Canada, provinces and territories. Statistics Canada. February 9, 2022. Accessed August 6, 2024. https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=9810000101
Newsletter
Where clinical, regulatory, and economic perspectives converge—sign up for Center for Biosimilars® emails to get expert insights on emerging treatment paradigms, biosimilar policy, and real-world outcomes that shape patient care.
