- Bone Health
- Immunology
- Hematology
- Respiratory
- Dermatology
- Diabetes
- Gastroenterology
- Neurology
- Oncology
- Ophthalmology
- Rare Disease
- Rheumatology
Opinion: A Short History of Biosimilars
Biosimilars have come a long way, and their path has mirrored that of generics—fraught with obstacles. Still, a stronger embrace is needed from physicians and payers.
The foundations for generics and biosimilars were laid in the enactment of several key pieces of legislation. In 1962, the Kefauver-Harris Amendments required proof of a product’s safety and efficacy, and they mandated that drugs released between 1938 and 1962 be reviewed for safety. In the late 1960s, the FDA developed the abbreviated new drug application for approval of generic drugs. The Drug Price Competition and Patent Term Restoration Act of 1984 (aka Hatch-Waxman) allowed the FDA to approve applications to market generic versions of brand-name drugs that were released after 1962 without repeating efficacy and safety studies; it also gave manufacturers of originator drugs 5 years of exclusivity for new products that contain previously unapproved chemical entities.
Originator drug companies were opposed to the idea of generic drugs and declared that these copycat drugs would cause havoc to health care. The protests were unsuccessful, and many of these manufacturers ultimately made generic drugs as well, although generics were less profitable for them.
History Repeats Itself
Now, 37 years after Hatch-Waxman, despite widespread use of generic drugs, the controversy continues about their safety and efficacy, particularly in prescribers’ minds. In 2010, the Biologics Price Competition and Innovation Act (BPCIA) was signed into law, and we saw history repeating itself as originator companies objected to biologics, as they had once objected to generics. However, this time, they found a sympathetic audience because the stakes were much higher. The most common argument presented was that biological drugs do not have a fixed structure, and manufacturing process controls are pivotal to assuring safety and efficacy. Because only innovator producers are privy to these controls, they contended, it is impossible to create a safe and effective copy of a biological drug.
AbbVie protested to the FDA in a citizen petition that the BPCIA constitutes an unlawful taking of private property under the Fifth Amendment because each biologics license application (BLA) contains trade secrets and confidential commercial or financial information, and the “approval of a biosimilar necessarily relies on and uses the trade secrets that the innovator sponsor submitted in support of the BLA.”1 The petition was denied by the FDA.
Many more petitions demanded that within biosimilar product labeling should be a declaration acknowledging that a biosimilar is different from the reference product. Extended lobbying efforts, as well, were aimed at getting state legislatures to preemptively ban interchangeable biosimilars. When originator companies realized that biosimilars were not going away, however, they got aboard the train, just as they did for the generic drugs. Big-name companies with many original biologics became the largest producers of biosimilars. Of 29 biosimilars so far approved by the FDA, all but a few are owned by the larger pharmaceutical companies. It might be assumed that the distrust sowed against biosimilars’ safety and efficacy by major pharmaceutical manufacturers would have dissipated, but it did not. Patients were reluctant to use these agents. And the same companies that once revolted against biosimilars adopted a new mantra: “Only we know how to make biosimilars because only we know how to make biological drugs.”
Physicians get information about new drugs from medical journals, continuing education meetings, and, most important, from visits by medical reps who are employed by the pharmaceutical industry. Physicians are good at what they do, but they are not scientists. They are well able to understand the results of a published clinical study, but most would be lost in the jungle of protein structure and immunogenicity profiling that is critical for biosimilar approval. Overall, the message received by physicians was simple: “Do not risk your patients.” The FDA did a lot to educate every stakeholder, including the physicians, but that was not enough to fully counter the bias created against biosimilars.
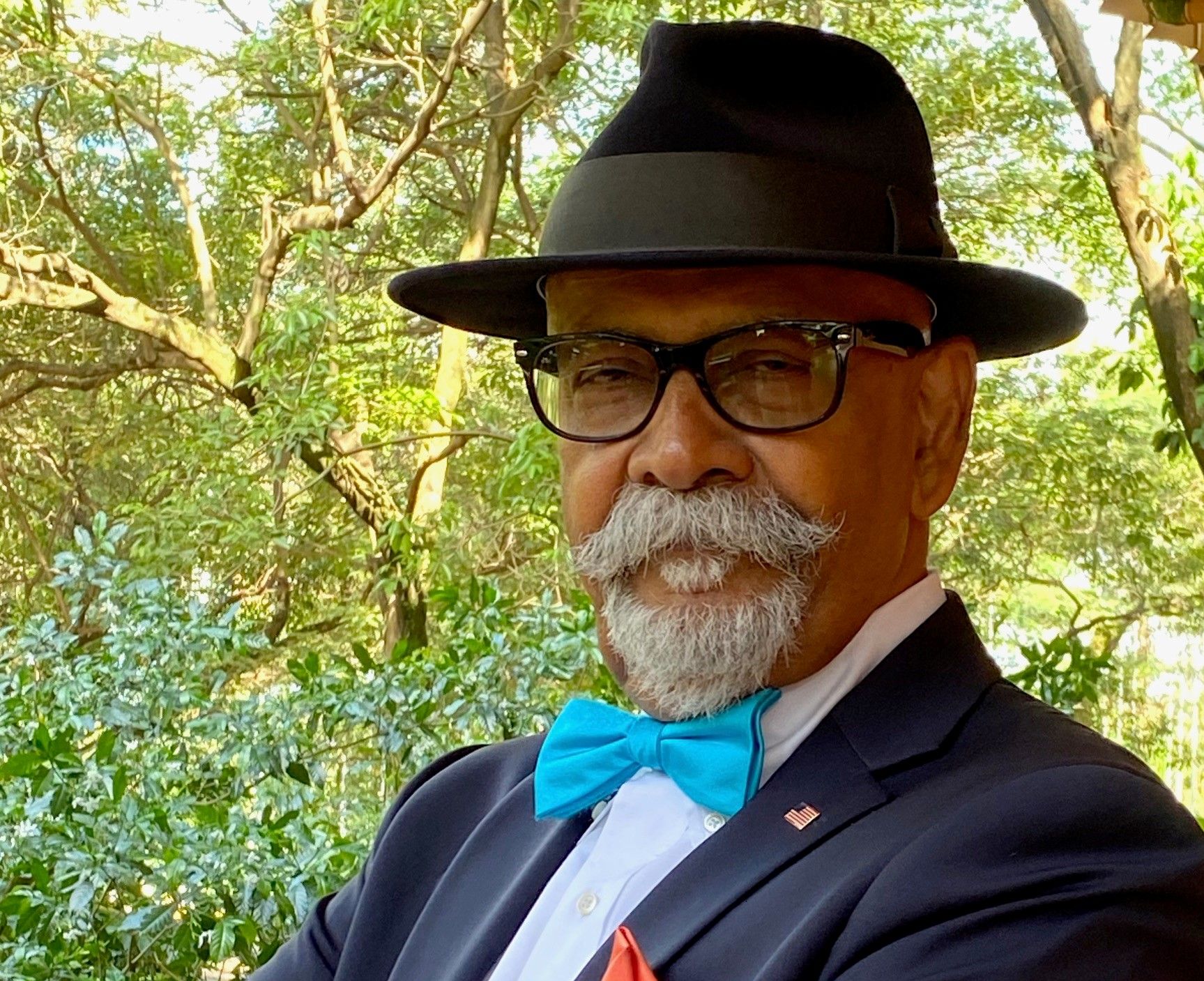
Over my career, I have conducted many advisory board meetings with stakeholders to introduce biosimilars. In 2019, I was hired by an originator company to educate physicians about biosimilars. To one group of about 500 primary care physicians, I presented a high school–level science lecture on biosimilars, with graphics, to reduce the jargon and complexity. Before my talk, I asked them to take a survey that included 2 questions: (1) Do you trust the safety and efficacy of biosimilars? and (2) Do you trust the FDA? Most physicians did not believe that biosimilars are safe, despite the FDA labeling that biosimilars in comparison with originator drugs have “no clinically meaningful difference” In response, I asked why they believed the FDA would not be truthful about biosimilars. The typical response was that, every year, many drugs are recalled and many companies are given citations for lack of current good manufacturing practice compliance. I had difficulty connecting these issues with the biosimilar issue, but the responses helped me understand the provider mindset: The FDA cannot assess the safety of biological drugs because if you do not know what you are looking for, how would you know you are not finding it?
Later, I gave these physicians another survey that asked these questions: (1) Would you prescribe a biosimilar to a patient if the insurance will not pay for the originator product? and (2) Would you trust biosimilars from smaller companies, now that the innovator companies are also making biosimilars? To the first question, the answer was an overwhelming yes. And to the second question, it was overwhelmingly no. I did not get a chance to continue my arguments. Still, in a social gathering over lunch, many physicians agreed that they did not have the time to understand the scientific nuances I presented in my talk. In brief, physicians remain misinformed or ill-informed about the FDA’s role in assuring the safety and efficacy of drugs, and originator companies perpetuate the confusion by asserting it is only a published clinical trial of efficacy that matters.
One physician was very frank. Her hospital has a policy of using biosimilars where available, and prescribers can get approval for an innovator biologic only by filling out a 10-page form. That killed the revolt against biosimilars quickly, she said.
Getting Physicians and Payers Aboard
So, where do we go from here to make physicians believe in biosimilars? The first responsibility goes to the FDA. Often, physicians do not scroll the pages of FDA websites or watch FDA YouTube videos. My suggestion to FDA Acting Commissioner Janet Woodcock, MD, is that she send a direct communication to physicians (a paper letter, not an email) to assure them that when the FDA approves a biosimilar, that is a golden seal of “no clinically meaningful difference.”
Second, payers can do their part to increase biosimilar use by establishing reimbursement policies that favor biosimilars, a sure-fire means of getting lower-cost biosimilars into play. I have also met with CMS leaders and suggested a legislative change to enable CMS to create a biologics substitution list that is based on cost with no other differentiation between a biosimilar and a reference product. This has already been tried in Europe; it works and will work in the United States.
Third, biosimilar developers should monitor misleading or anticompetitive public statements made about biosimilars and report these to the FDA and Federal Trade Commission. Innovator companies have been admonished for such actions by regulators before. Merely reaching out to physicians to explain the advantages of biosimilars may not be enough if entities opposed to biosimilars continue to disparage these agents.
With proper, unhindered education about the value of biosimilars, these cost-saving agents can become as significant a force in improving access to health care as generics have before them.
Reference
Regulations.gov. Citizen petition from AbbVie, Inc. FDA. Published June 3, 2015. Accessed February 16, 2021. https://www.regulations.gov/document?D=FDA-2015-P-2000-0001
Newsletter
Where clinical, regulatory, and economic perspectives converge—sign up for Center for Biosimilars® emails to get expert insights on emerging treatment paradigms, biosimilar policy, and real-world outcomes that shape patient care.