- Bone Health
- Immunology
- Hematology
- Respiratory
- Dermatology
- Diabetes
- Gastroenterology
- Neurology
- Oncology
- Ophthalmology
- Rare Disease
- Rheumatology
Part 3: Study Questions Usefulness of Clinical Efficacy Trials for Oncology Biosimilars in Europe
In part 3 of a 3-part series for Global Biosimilars Week, The Center for Biosimilars® reviews an analysis investigating whether clinical efficacy studies have an impact on prescribing decisions for oncology biosimilars across Europe.
Click to enlarge.
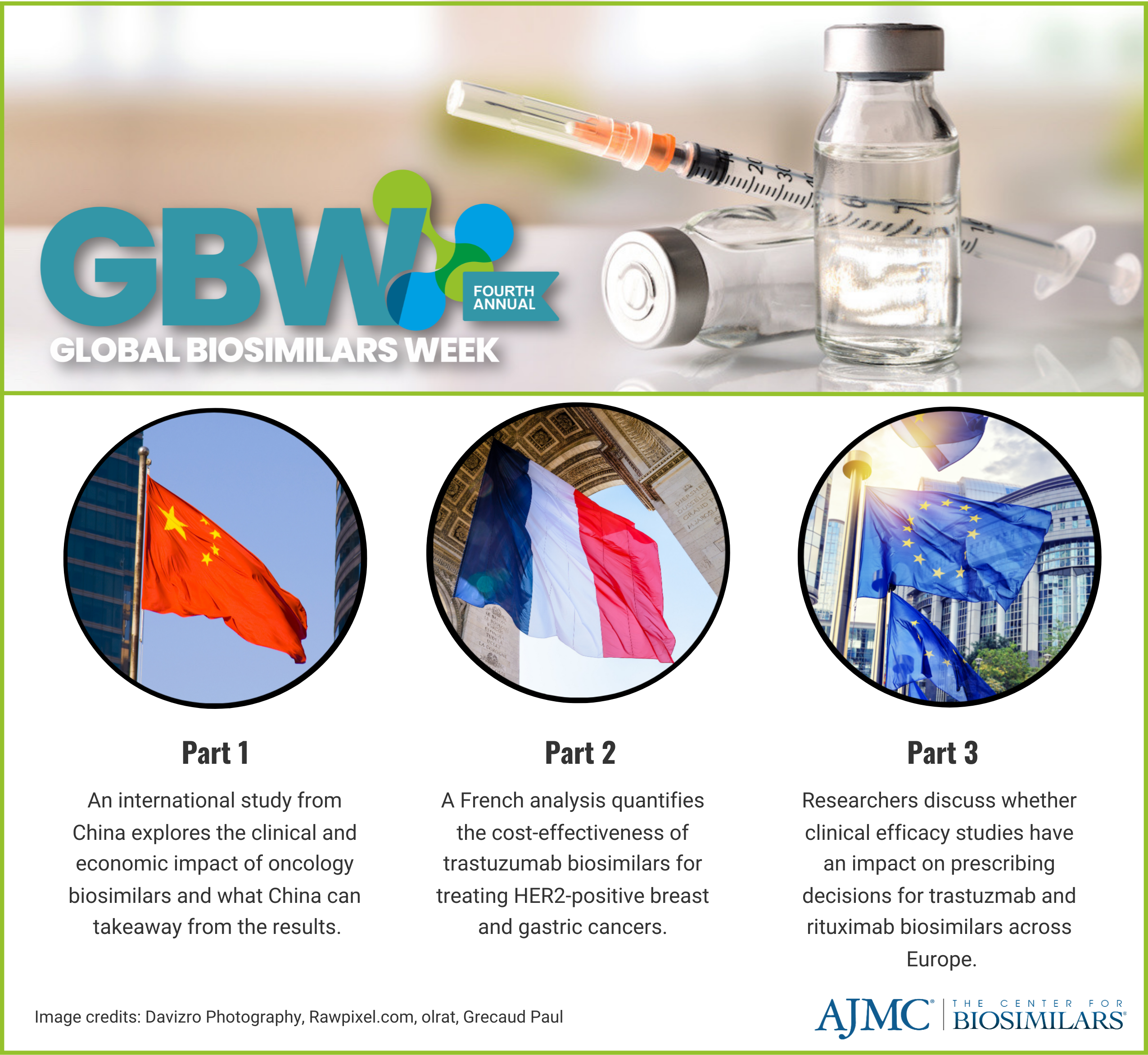
In part 3 of a 3-part series for Global Biosimilars Week, The Center for Biosimilars® reviews an analysis investigating whether clinical efficacy studies have an impact on prescribing decisions for oncology biosimilars across Europe.
Global Biosimilars Week is an annual awareness campaign created by the International Generic and Biosimilar Medicines Association. The event runs from November 13-17, 2023, and serves as a way to expand awareness of biosimilars, their clinical effects compared with originators, the economic impacts of using them, and the growing industry worldwide. To read part 1, click here. To read part 2, click here.
The present study, published in BioDrugs, was conducted to analyze the role of quality/chemistry, manufacturing and controls (CMC), and clinical data for the conclusion on biosimilarity and the decision on marketing authorization. The analysis also highlighted the need for a comprehensive approach that includes both quality/CMC and clinical data to ensure patient safety and efficacy of biosimilars.
Over the past 5 years, the global biosimilars market has greatly matured; however, between 2023 and 2027, estimates show that 55% of biologics losing patent exclusivity do not have biosimilar competitors coming down the pipeline. Development costs for biosimilars can range from $100 million to $300 million, much larger than the costs to develop a small molecule generic.
“Products with low sales value are unattractive to biosimilar manufacturers due to clinical development costs, largely driven by large and lengthy clinical trials and procurement costs of reference product (RP) comparator batches…. This cannot be in the interest of stake- holders, including regulators, and contradicts the strategic priorities of the European Medicines Agency (EMA), which has set out to allow for more rational use of clinical resources,” the authors wrote.
Although there are some initiatives to impact regulatory decision-making and revised guidelines have launched, including efforts to omit or reduce the number of human participants required for clinical trials in more cases, questions remain on whether biosimilar candidates with promising preclinical data could translate to poor or failed clinical trials, which can prevent regulatory approval.
The researchers assessed the data submitted as part of marketing authorization applications (MAAs) of the 36 monoclonal antibodies (mAbs) and fusion protein biosimilars evaluated by the EMA from July 2012 to November 2022—including withdrawn applications (n = 2)—with special emphasis on the 4 rituximab and 7 trastuzumab biosimilar candidates. Withdrawn applications, where comparative efficacy trials suggested biosimilarity between the biosimilar and originator but the EMA did not accept the quality/CMC package, the authors evaluated whether quality/CMC data could predict a negative MAA outcome, regardless of clinical trial data.
In 67% of cases, the quality and clinical assessments supported approval or did not support approval. In 11% of cases, issues were found in the quality part but not in the clinical data. In 22% of cases, problems were identified in the clinical data but not in the quality data.
Notably, the study revealed consistent high similarity in critical quality attributes for biosimilars of rituximab and trastuzumab, with over 90% of batches meeting the EU reference product similarity range. This underscores the robustness of the quality/CMC package, which successfully resolved uncertainties without relying on clinical trial data, emphasizing its ability to predict clinical outcomes.
Within comprehensive clinical programs for rituximab and trastuzumab biosimilar candidates, the researchers identified redundancy in pharmacokinetic (PK) evaluations, suggesting potential streamlining opportunities, especially considering the specific binding mechanism of rituximab. The study also highlighted regulatory flexibility, showcasing variations in primary end points and equivalence margins within accepted clinical data packages.
The researchers concluded that a robust analytical/functional similarity package, along with a PK trial capturing safety and immunogenicity data, could suffice for regulatory decision-making on biosimilar mAbs and fusion proteins. Additionally, the study raised questions about the necessity of extensive analyses of secondary end points in efficacy trials. Interestingly, the findings indicated that preliminary data submitted during the evaluation period remained consistent with conclusions reached after the full 1-year dataset submission, suggesting the potential redundancy of long-term trials.
However, the analysis also noted no cases where negative clinical data led to an overall negative decision, attributing discrepancies to factors such as trial imbalances and changes in the reference product, as detailed in the evaluation of trastuzumab and rituximab biosimilars.
The study, centered on immunoglobulin G class mAb and fusion protein biosimilars, has limited applicability to more complex biologics, focuses on regulated products, and may overlook biosimilars not reaching regulatory evaluation. With a sample size of 36 from the last decade's EMA submissions, this study included the largest set analyzed to date.
“These findings allow a reduction of the clinical development program for regulatory review before MA. This conclusion is further supported by the positive experience in the market gained for biosimilar mAbs approved in the last 10 years. Consequently, a revision of the respective regulatory biosimilars guidelines in Europe should be considered, to allow a more rational use of clinical resources and improve the access to innovative and affordable medicines for patients."
Reference
Kirsch-Stefan N, Giullen E, Ekman N, et al. Do the outcomes of clinical efficacy trials matter in regulatory decision‐making for biosimilars? BioDrugs. 2023;37(6):855-871. doi:10.1007/s40259-023-00631-4
Newsletter
Where clinical, regulatory, and economic perspectives converge—sign up for Center for Biosimilars® emails to get expert insights on emerging treatment paradigms, biosimilar policy, and real-world outcomes that shape patient care.
