- Bone Health
- Immunology
- Hematology
- Respiratory
- Dermatology
- Diabetes
- Gastroenterology
- Neurology
- Oncology
- Ophthalmology
- Rare Disease
- Rheumatology
Physicians Agree on Safety of Biosimilars, Nonmedical Switching in IBD, Survey Says
An international survey found that providers agree that use of biosimilars in inflammatory bowel disease (IBD) is safe and effective in both patients who are treatment-naïve and those who are already being treated with a reference agent.
A global survey of physicians treating inflammatory bowel disease (IBD) found consensus that biosimilars are a promising option for improving patient access to highly effective treatments for IBD, while reducing health care costs and maintaining improved health outcomes.
The paper, published in the Journal of Clinical Medicine, provided practical guidance for health care professionals on the use of biosimilars in IBD treatment, including recommendations for initiating, transitioning, and switching between biosimilars. However, the study acknowledged the need for further research and education to address remaining concerns and challenges related to biosimilar adoption.
To ensure that biosimilars can serve as a cost-effective alternative to originator biologics within health systems, addressing various challenges in clinical management of IBD remains crucial. The researchers wanted a better understanding of physicians’ current knowledge, beliefs, practical approaches, and concerns related to biosimilar adoption. The also wanted to gather insight into provider apprehensions about initiating a biosimilar treatment, including their feeling about transitioning from an originator to a biosimilar, or switching between biosimilars (multiple switches and reverse switches).
A cross-sectional survey with 46 questions was conducted from January to February 2023 using an online platform. Responses were collected anonymously, and the questions were multiple-choice and only offered in English. The questions focused on 5 areas:
- Participant demographics, specialty, and level of experience
- Practices and attitudes toward biosimilar use in clinical practice
- Concerns about interchangeability, including reverse and multiple switches
- Concerns about the nocebo effect and nonmedical switch
- Current and future perspectives
In total, 234 providers from 38 countries responded to the survey, of whom 39% were aged 30 to 40 years and 43.6% were women. By expertise, 202 respondents were gastroenterologists, 6 were surgeons, 3 were medicine specialists, 3 were general practitioners, and 20 were other specialists. Most participants had over 10 years of experience working with patients with IBD.
Over 80% of respondents (n = 195) believed biosimilars were as safe and effective as originator drugs. The participants rated their own confidence in biosimilars as moderate and their patients’ confidence as slightly lower (average rating from 0 to 10: 8.5 vs 7.7, respectively). Approximately 75% of respondents said that biosimilar data from other immune-mediated inflammatory diseases are valid and applicable to IBD, showing confidence in extrapolated indications.
Many providers had concerns about interchangeability and the nocebo effect. The survey found that many providers had difficulty defining terms like extrapolation and interchangeability in the context of biosimilar regulation, and many had a poor ability to articulate the differences between biosimilars and originators. Additionally, most providers were familiar with the concept of the nocebo effect, but approximately one-third could not confirm whether their patients had ever experienced it. When physicians were aware of the nocebo effect in their patients, in most cases, they believed it affected less than 5% of them.
Additionally, most health care practitioners believed that the availability of biosimilars would influence therapeutic choices, and more than half of IBD specialists had patients undergoing nonmedical switching.
Designed by Kyle Munz, Editor
Furthermore, most providers believed they would soon be prescribing biosimilars of vedolizumab and ustekinumab, as well as generics of small molecules. The study also found that the majority of respondents believed that the implementation of biosimilars in clinical practice requires more long-term data and randomized clinical trials to compare the biosimilarity of biosimilars and originator drugs in patients with IBD.
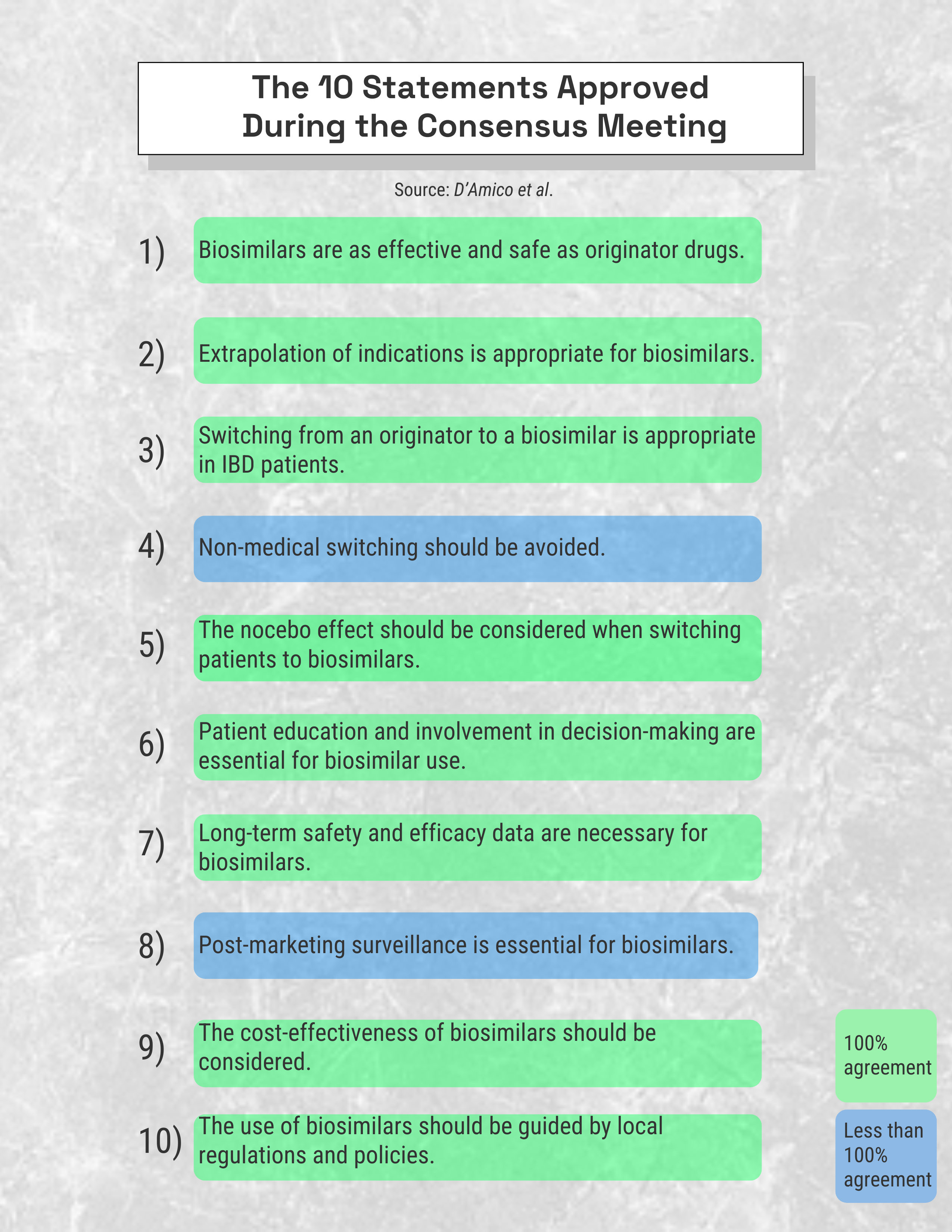
On February 21, 2023, a virtual consensus meeting including 15 providers who treat IBD from 13 countries (Argentina, Brazil, Canada, France, Germany, Ireland, Italy, Japan, Portugal, Spain, Sweden, United Arab Emirates, and United States). As a result, 11 statements were formulated and anonymously voted on by all participants using Delphi consensus methodology through a virtual platform. The statements were approved if at least 75% of participants reached a consensus (n = 10). Of the 10 approved statements, 100% agreement was reached for 8. (Figure)
“The present survey provides insights regarding IBD specialists’ practical management, beliefs, and knowledge surrounding biosimilars. The subsequent consensus provides guidance for the development and use of biosimilars in IBD treatment, based on the insights and perspectives of a global panel of experts,” the authors concluded.
Reference
D’Amico F, Solitano V, Magro F, et al. Practical management of biosimilar use in inflammatory bowel disease (IBD): a global survey and an international Delphi consensus. J Clin Med. 2023;12(19):6350. doi:10.3390/jcm12196350
Newsletter
Where clinical, regulatory, and economic perspectives converge—sign up for Center for Biosimilars® emails to get expert insights on emerging treatment paradigms, biosimilar policy, and real-world outcomes that shape patient care.
