- Bone Health
- Immunology
- Hematology
- Respiratory
- Dermatology
- Diabetes
- Gastroenterology
- Neurology
- Oncology
- Ophthalmology
- Rare Disease
- Rheumatology
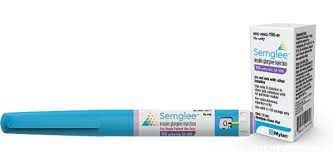
Prime Therapeutics Joins Express Scripts in Moving Semglee to Preferred Formulary Status
Prime Therapeutics said that by putting Semglee (insulin glargine) on formulary, along with other biosimilars, it could achieve savings of $41 million or more per year.
Prime Therapeutics, a large pharmacy benefit manager (PBM) with 33 million Blue Cross and Blue Shield plan members, said it will put the insulin glargine biosimilar Semglee on its preferred formulary.
Semglee was approved as an interchangeable biosimilar by the FDA in July 2021, and Prime’s decision to promote use of this agent follows a similar decision in October by Express Scripts, another PBM, which put the agent on its largest national formulary.
Semglee was originally launched in August 2020 by Biocon Biologics and Mylan (now Viatris) but did not obtain biosimilar and interchangeable status until July 2021. Interchangeability means the drug can be switched for the reference product (Lantus) at the discretion of the pharmacist.
"This formulary change reinforces Prime's commitment to increasing biosimilar adoption and also demonstrates that we are not beholden to rebates, as we're able to also prefer the lowest net cost therapy," Kelly Pokuta, vice president and chief trade relations officer for Prime, said in a statement.
Rebates and discounts offered by manufacturers often cloud the pricing picture for biosimilars and reference products, so it’s often unclear to the public which is the lower-priced agent and how much the agent is actually selling for.
"No Disruption"
The PBM vowed in its statement that there would be “no significant member disruption and affordability will be comparable or better with the biosimilar.” The formulary placement would take effect on January 1, 2022.
Semglee is the only insulin glargine product that is available in biosimilar or interchangeable form currently in the United States.
There is a pipeline of insulin products that are expected to debut as biosimilars in the near future, posing competition for dominant reference brands, which have maintained often stubbornly high and increasing prices to the detriment of affordability and access, such that insulin prices have become a hot-button issue for patients and patient advocates.
Biosimilars in other therapeutic classes have been competing successfully with reference products and bringing down prices. Prime acknowledged this in its statement: “Biosimilars often have initial prices that are 15% to 35% lower than the reference products, which is particularly important as drug costs continue to increase, and specialty drugs now represent more than 50% of the health care dollar.”
The placement of Semglee on formulary follows a recent Prime announcement that it would increase management of claims to drive broader biosimilar adoption via the launch of a program called “MedDrive.”
“The first phase focuses on drug savings strategies through greater biosimilar drug adoption, most of which are paid on the medical benefit,” the PBM said. “Other elements of the initial program include benefit designs that prefer lowest net cost nonbiosimilar drugs.”
The company contended that “a fragmented approach to managing drugs under the medical benefit” is responsible for obstructing greater adoption of biosimilars.
G-CSF Biosimilar Savings
Prime stated in a recent white paper that its experience with granulocyte colony-stimulating factor (G-CSF) biosimilars and reference products has convinced it that moving biosimilar promotion “into high gear” through preferential formulary strategies is the way to go.
In September 2018 the PBM experimented with G-CSF biosimilars by preferring them in 3 Blue Plan client groups and placing them on equal formulary status with other Blue Plan groups. The result was that the biosimilar preferential policies resulted in significantly higher biosimilar conversion rates (87%, 88%, and 98%, respectively) than for the non–G-CSF biosimilar preferring plans (average, 24%).
“Adding biosimilars to the formulary and preferring them, for even just 3 plans, collectively delivered savings of $4 million in 2019,” Prime said. “If all Prime’s Blue Plan clients prefer biosimilars in the G-CSF space and adoption rates follow, we project savings of $41 million to $55 million a year.”
Newsletter
Where clinical, regulatory, and economic perspectives converge—sign up for Center for Biosimilars® emails to get expert insights on emerging treatment paradigms, biosimilar policy, and real-world outcomes that shape patient care.