- Bone Health
- Immunology
- Hematology
- Respiratory
- Dermatology
- Diabetes
- Gastroenterology
- Neurology
- Oncology
- Ophthalmology
- Rare Disease
- Rheumatology
Study: Grastofil Equivalence Confirmed in ASCT Setting
A Canada study of the filgrastim biosimilar Grastofil demonstrated equivalence to Neupogen in candidates for autologous stem cell transplantation (ASCT), an extrapolated use.
Investigators in Canada reported positive comparative findings for filgrastim biosimilar use in promoting stem cell regeneration in patients with hematological malignancies. They said the evidence supports the extrapolated use of biosimilars across indications approved for originator drugs.
The filgrastim biosimilar Grastofil was studied in the context of mobilization and engraftment, or stimulated movement of stem cells from bone marrow for collection, storage, and later use to replace bone marrow cells (autologous stem cell transplantation, ASCT) that have been damaged by chemotherapy and radiation (myeloablation).
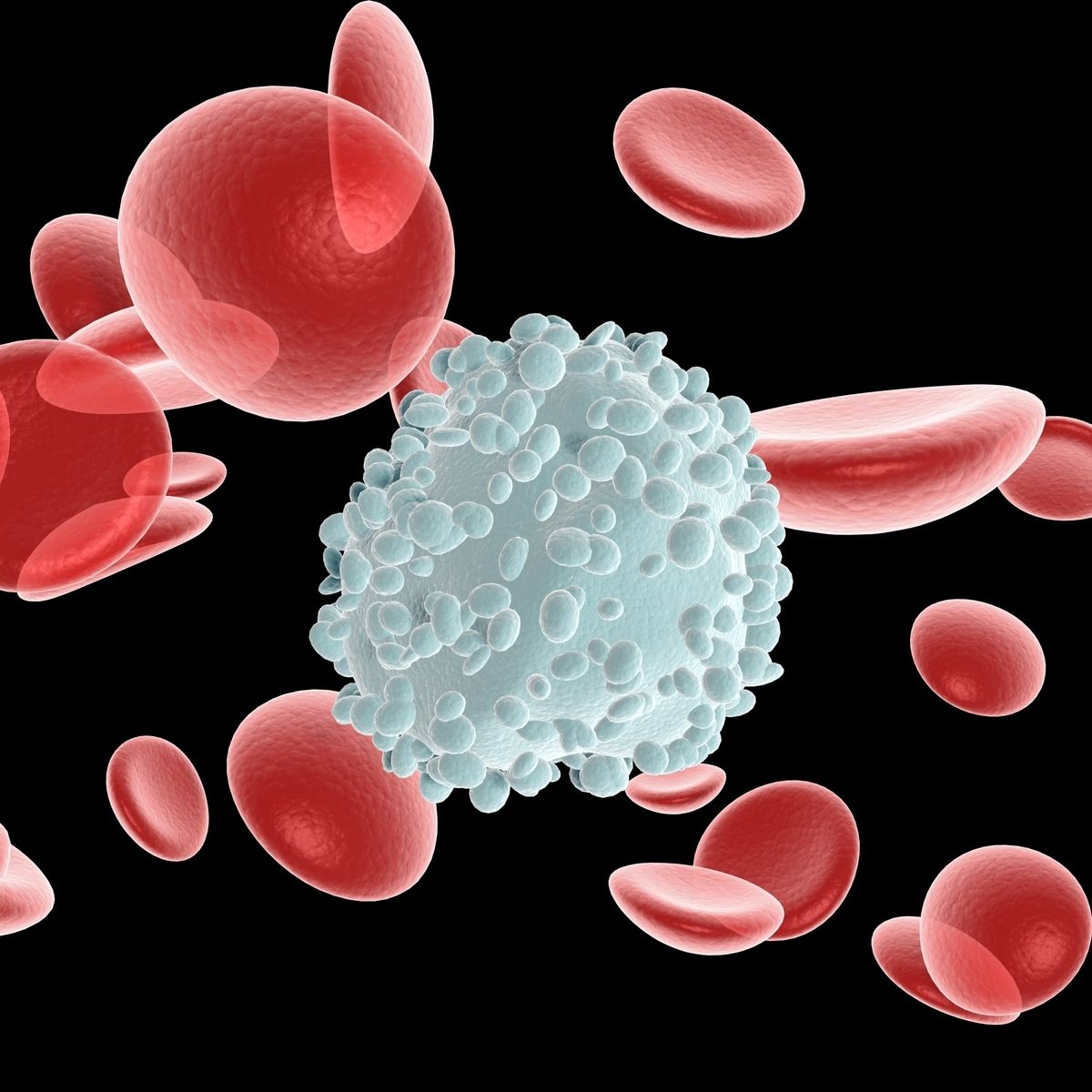
Filgrastim promotes immune cell production and is the first-line treatment for stem cell mobilization in patients with hematological malignancies who receive myeloablative therapy followed by ASCT, the authors wrote.
The real-world study comparing the biosimilar granulocyte colony-stimulating factor (G-CSF) to its reference product filgrastim (Neupogen) for stem cell mobilization prior to ASCT reported similar CD34+ peripheral blood stem cell collection success rates, engraftment kinetics, and hospital stay periods.
In 2016, the Saskatchewan Cancer Agency made a switch from the originator filgrastim to Grastofil, the first biosimilar G-CSF approved in Canada, for all indications of the originator drug. However, the authors noted that because data for patients undergoing stem cell mobilization prior to ASCT were scarce, “physician hesitancy prompted many institutions to continue relying upon higher priced originator products.”
The researchers conducted a retrospective chart review of data from The Saskatchewan Cancer Agency. They identified 217 patients who underwent stem cell mobilization and transplant between 2012 and 2018. Of those, 170 were treated with the reference product before the 2016 switch, and 47 with the biosimilar after. The authors noted “there were no significant changes in the mobilization [procedure] practiced at this institution” across the 2 time periods. They also mentioned that patients treated with the biosimilar were somewhat older (mean age 59.3 years) than those treated with the reference product (55.9 years).
The primary end point was successful CD34+ stem cell harvest, and investigators reported a 100% success rate in patients receiving the biosimilar and 92.4% in those receiving the reference product; the difference was not statistically significant (P = .075).
In cases of low peripheral CD34+ count the day before the scheduled collection, plerixafor (Mozobil) was used as a supplemental therapy to increase stem cell mobilization. Rates of plerixafor use were similar in the reference product and biosimilar groups (25.9% and 23.4%, respectively; P = .72).
Among patients mobilized with the biosimilar, 59.6% required more than 1 apheresis day compared with 48.8% of those treated with the reference product, a difference that was not statistically significant (P = .19).
Engraftment was assessed based on absolute neutrophil count (ANC) recovery and platelet recovery, both of which were described as “highly similar” between groups by the researchers. Mean ANC recovery time in both groups was 11.6 days, and mean platelet recovery time was 14.0 days in patients treated with the reference product vs 14.2 days for the biosimilar. Mean total hospital stay lengths was also similar: 22.4 days for the reference product vs 22.3 days for the biosimilar.
Investigators did not detect any significant differences between groups in these outcomes with further analyses based on disease type or use of chemotherapy. They acknowledged their study did not evaluate safety outcomes.
The authors said their real-world data “built upon other real-world evaluations of biosimilar G-CSF products in the ASCT mobilization setting to help extend global evidence supporting confidence in using biosimilar G-CSF across all approved indications.” They also stressed the significance of their study as “one of the first real-world evidence studies using biosimilar G-CSF in the ASCT setting in Canada.”
Reference
Aggarwal V, Sabry W, Elemary M, et al. Real world clinical experience of biosimilar G-CSF (Grastofil) for autologous peripheral blood stem cell mobilization: single center experience in Canada following early adoption. Curr Oncol. 2021;28(3):1571-1580. doi:10.3390/curroncol28030148
Newsletter
Where clinical, regulatory, and economic perspectives converge—sign up for Center for Biosimilars® emails to get expert insights on emerging treatment paradigms, biosimilar policy, and real-world outcomes that shape patient care.