- Bone Health
- Immunology
- Hematology
- Respiratory
- Dermatology
- Diabetes
- Gastroenterology
- Neurology
- Oncology
- Ophthalmology
- Rare Disease
- Rheumatology
Switch to Biosimilar BAT1806/BIIB800 Maintains Efficacy, Safety in Patients With RA
Switching to the biosimilar version of tocilizumab (BAT1806/BIIB800) showed similar effectiveness, safety, and tolerability compared with the original drug for patients with rheumatoid arthritis (RA) who had an inadequate response to methotrexate.
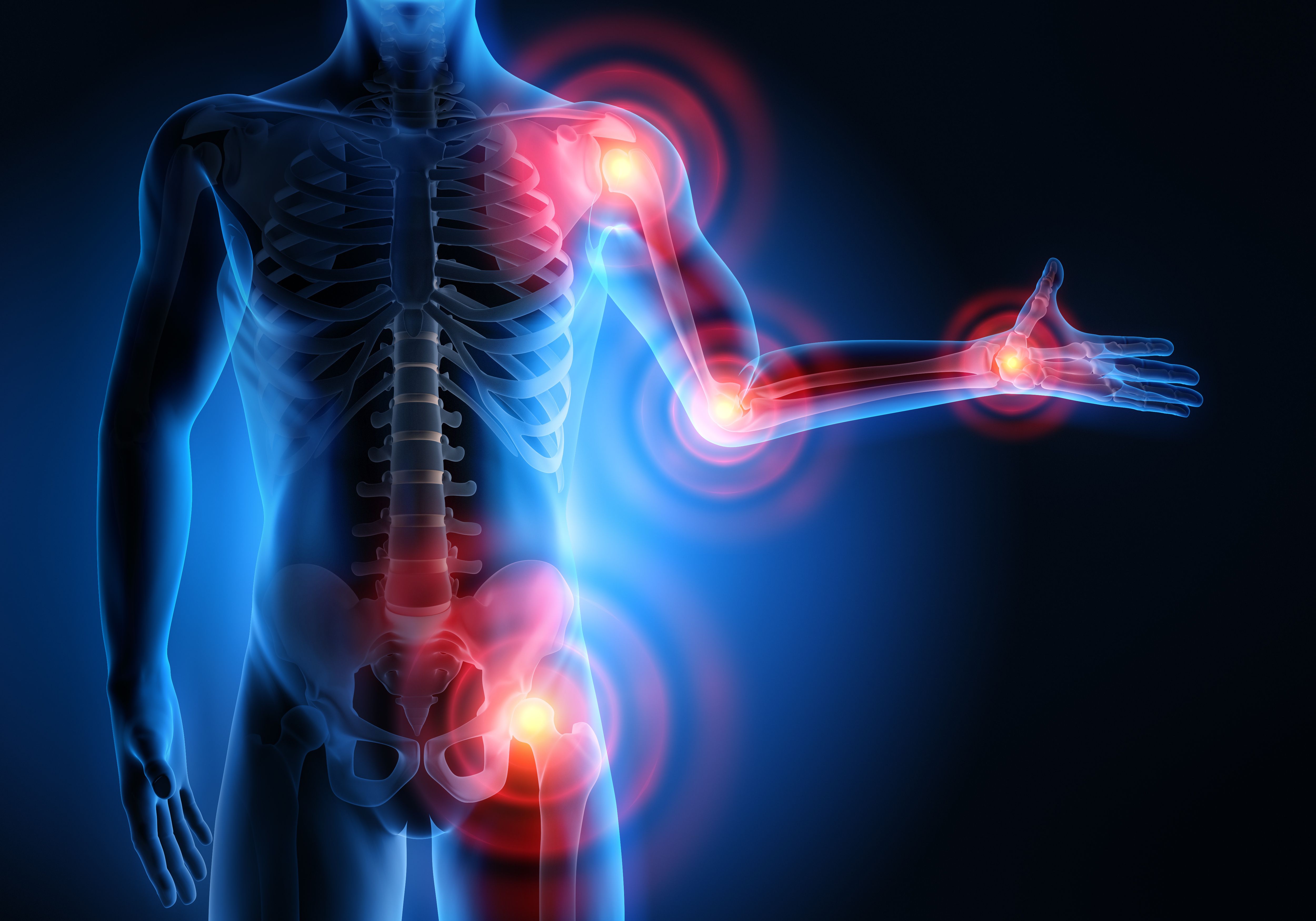
Inflamed areas affected by rheumatoid arthritis | Image Credit: peterschreiber.media - stock.adobe.com
Patients with rheumatoid arthritis (RA) that did not respond well to methotrexate experienced no difference in efficacy, safety, immunogenicity, or pharmacokinetic (PK) profiles when they switched to the proposed tocilizumab biosimilar, BAT1806/BIIB800.
In a phase 3, multicenter, randomized, double-blind, active-controlled, equivalence study conducted from December 19, 2018, to January 5, 2021, examined participants in a 24-week initial treatment period followed by a 24-week secondary treatment period (48 weeks). Patients were recruited from 54 centers across China, Ukraine, Poland, Georgia, and Bulgaria.
Participants were assigned at random through a computerized, interactive, web-response system to receive reference tocilizumab up to week 48, reference tocilizumab up to week 24 followed by BAT1806/BIIB800 up to week 48, or BAT1806/BIIB800 up to week 48.
Study demographics were similar between originator tocilizumab and biosimilar BAT1806/BIIB800 (n = 309, 312, respectively). Both groups had a majority of White, female participants from central Europe.
Medication was administered once every 4 weeks at an 8 mg/kg dose by a 1-h intravenous infusion up to and including week 20. A stable 10 to 25 mg dose of methotrexate therapy per week continued among all participants. The Disease Activity Score in 28 joints (DAS28) and individual response rates based on the American College of Rheumatology (ACR) were utilized as study resources.
Aside from RA, common conditions among patients were hypertension, menopause, osteoporosis, and anemia (26%, 13%, 10%, 9%). Treatment period 1 was completed by 93% of participants in both the reference and tocilizumab biosimilar group.
The primary endpoint was measured as the proportion of participants with a 20% (ACR20) improvement based on the ACR criteria by week 12 or 24. An estimated proportion of participants with an ACR20 response were 64.8% in the reference group and 69.0% in the biosimilar at week 12 and 67.9% in reference group and 69.9% in biosimilar group at week 24. The estimated difference between ACR20 response rates was 4.1% at week 12 and 1.9% at week 24. Both groups consisted of comparable PK and immunogenicity profiles.
From baseline to week 24, neither group expressed major differences in proportions of ACR20, ACR50, ACR70 or in the number of respondents over time. Baseline reductions were similar in the DAS28-erythrocyte sedimentation rate and DAS28-C–reactive protein among groups.
A total of 407 participants experienced about 1340 adverse events (AEs) throughout treatment period 1, mainly of mild severity. The reference group consisted of 151 patients with treatment emergent adverse events (TEAEs) and 140 patients made up the BAT1806/BIIB800 group. Infections were the most common serious TEAEs, reported in 5 of the participants in the reference group and 3 of the patients taking BAT1806/BIIB800. Only 1 fatal event was reported as potentially related to the medications.
Safety profiles of reference tocilizumab and BAT1806/BIIB800 were comparable but had lower risk of infections in the biosimilar group. No meaningful differences in PK among treatment groups were measured by serum trough levels with variability observed in both groups.
Study limitations were caused by the majority of European women enrolled in both groups without including radiographic assessments as a measure of disease progression.
Patients with RA that had inadequate responses to methotrexate expressed equivalent efficacy of BAT1806/BIIB800 to the EU-sourced reference tocilizumab over a 48-week treatment period with the COVID-19 pandemic concluding little to no effect on the study conduct.
Reference
Leng X, Piotr Leszczyński, Jeka S, et al. Comparing tocilizumab biosimilar BAT1806/BIIB800 with reference tocilizumab in patients with moderate-to-severe rheumatoid arthritis with an inadequate response to methotrexate: a phase 3, randomised, multicentre, double-blind, active-controlled clinical trial. Lancet Rheumatol. 2024;6(1):e40-e50. Published Online Feb. 5, 2024. doi:10.1016/s2665-9913(23)00237-0
Newsletter
Where clinical, regulatory, and economic perspectives converge—sign up for Center for Biosimilars® emails to get expert insights on emerging treatment paradigms, biosimilar policy, and real-world outcomes that shape patient care.
